Compensatory Strategies for Cognitive Deficits
Related to Dementia
Problem: Dementia is a chronic, irreversible disorder of the mental processes caused by
damage to the brain. There are many forms of dementia including Alzheimer’s Disease (60%-
75% of dementia cases), Dementia with Lewy Bodies, Vascular Dementia, Parkinson’s Disease
Dementia, Frontotemporal Dementia, and Mixed Dementia (Barney, Emerita, & Perkinson,
2018). Onset of dementia is gradual and usually progresses over years. Additional information
can be found at https://www.healthline.com/health/dementia/early-warning-signs.
Initial signs of dementia often include:
Decreased short-term memory
Decreased visual-perceptual skills
Decreased problem-solving skills
Problems with language and
communication
Personality changes
An example of decreased short-term memory, or short-term
memory loss, could be forgetting names or appointments, but
remembering later. Another example is they can remember
an event that happened in their childhood but can’t
remember what they had for breakfast.
An example is having a harder time
distinguishing where steps are. It is
important to keep the environment
clutter free as vision changes and
perceptual deficits are common.
An example is making occasional mistakes when paying bills
or being unable to think through the next move when playing
a game. Problem solving skills help determine the source of
the problem and the solution for it.
An example is being repetitive due
to memory loss, such as repeating
the same questions that have
already been answered during a
conversation.
An example of a personality change would be to see a shift from
outgoing to shy. Depression is typically an early sign of
dementia. General behavioral changes, confusion, problems
with speaking/writing and loss of interests in hobbies are also
common.
The different types of dementia, listed above, lead to various symptoms in later stages of the disease.
Below is a short description of each type of dementia along with specified symptoms that are commonly
seen as the dementia progresses.
Alzheimer’s Disease (AD): Alzheimer’s is an age-related dementia which is more common in
women and accounts for 60% to 75% of dementia cases. It is most prevalent in those 65 and older and
there is currently no known cure for Alzheimer’s. Those with Down Syndrome are at a high risk of
developing this disease with symptoms becoming prominent at younger ages (40s and 50s).
Later symptoms: difficulty learning and recalling new information, and progressive language disorder
and trouble word finding. Short-term memory deficits leading to more evident memory loss and
disorientation in later stages. Inability to name objects will progress to inability to recognize familiar
objects and people (Barney, Emerita, & Perkinson, 2018). More information about Alzheimer’s disease
symptoms along with the stages associated with the progression can be found at
https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet#stages.
Dementia with Lewy Bodies (DLB): DLB is more common in males and accounts for 15% to 20%
of all older adult dementia cases (Barney, Emerita, & Perkinson, 2018). Symptoms of DLB vary
greatly from day to day. High-potency antipsychotic medications should be avoided as individuals with
DLB are highly sensitive them.
Later symptoms: Loss of ability to create new memories, increased confusion for days at a time,
changes in thinking and reasoning, visual hallucinations, delusions, slow walking/impaired balance,
fluctuation between being zoned out and fully alert, sleep disturbances and feeling tired or lethargic
during the day (even after getting enough sleep) are all common symptoms of DLB.
Vascular Dementia (VaD): The onset of vascular dementia is sudden, often associated with a stroke
or evidence of an infarct. As many as 30% of stroke survivors have dementia 6 months after; having a
stroke increases the risk of dementia by ninefold (Barney, Emerita, & Perkinson, 2018). Along with
strokes, VaD is also caused by having small vessels.
Later symptoms: Slowing signs in mental process, impaired judgement, personality changes, confusion,
difficulty concentrating, agitation, decreased language skills, urinary incontinence and visual
disturbances. Parkinsonian symptoms such as restlessness, shuffled gait, and loss of postural reflexes
are also commonly seen in those who have VaD.
Parkinson’s Disease Dementia (PDD): Often occurs in a person who has already had a
Parkinson’s diagnosis for at least a year. Up to 80% of those with Parkinson’s disease will develop
PDD (Barney, Emerita, & Perkinson, 2018).
Later symptoms: Resting tremors, slowed movements, soft voice, rigidity/stiffness of arms and legs,
masked facial expression, tiny handwriting, shuffled gait, and abnormal postural reflexes.
Frontotemporal Dementia (FTD): Second most common dementia in people under the age of 65.
Typically, there are a lack of neurological signs and symptoms upon initial diagnosis. FTD is
sometimes misdiagnosed for a psychiatric disorder (depression, bipolar, etc.) and corrected when
symptoms including memory deficits, balance problems, and stiffness progress.
Later symptoms: Slow onset of behavioral and personality changes, lack of insight, lack of emotion,
poor judgement, impolite behavior, loss of empathy for others, excessive weight gain, stubbornness,
compulsive behaviors, pacing, substance abuse, and social misconduct.
Mixed Dementia: Mixed dementia is common.
Later symptoms: Presentation of simultaneous symptoms of AD and VaD, AD and DLB, AD and PDD,
and VaD and DLB are possibilities.
Occupational Therapy Treatment Approaches
Although it is rare that cognitive performance improves, the person’s function
may improve when using adaptation or compensatory strategies.
https://www.aota.org/AboutOccupationalTherapy/Professionals/PA/Facts/Deme
ntia.aspx.
Compensatory strategies may be used for individuals to learn specific
methods and skills so they are able to compensate for areas there may be deficits.
For example, if Mary who is in the pre-dementia stage of Alzheimer’s Disease is
having a hard time remembering the times of her appointments, compensatory
strategies she may use could include making all her appointments at the same
time of the day. Another compensatory strategy for Mary could be to use a
calendar to keep track of her appointments where she could refer to her schedule
as often as she needed. More compensatory strategies include:
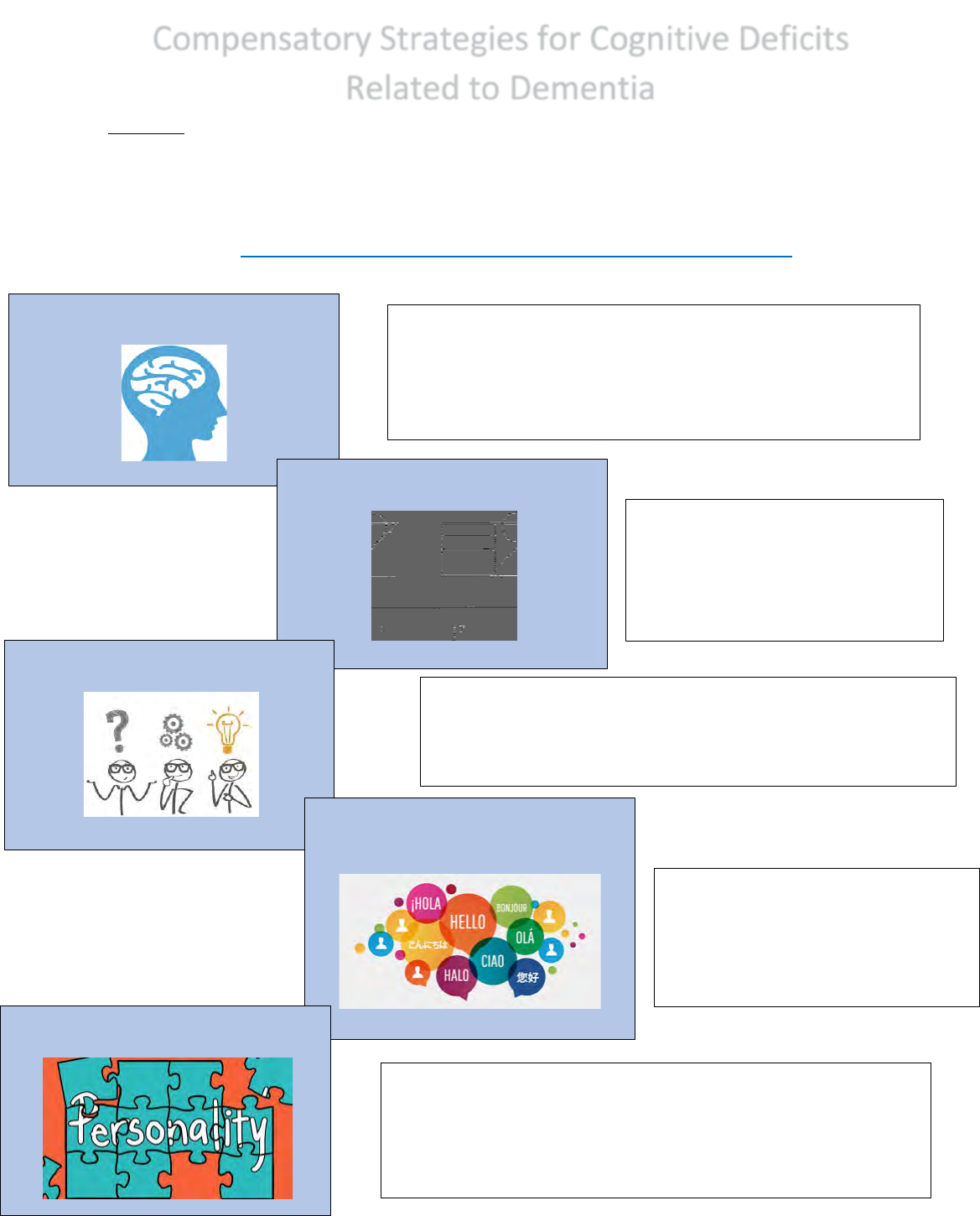
Appointments - Make
appointments and plans at
the same time of the day
Keeping phone/wallet in
the same place when not in
use
Make lists use sticky note
reminders
Keep a calendar
Organize daily pills in a pill
box
Use of assistive
technology
3
%
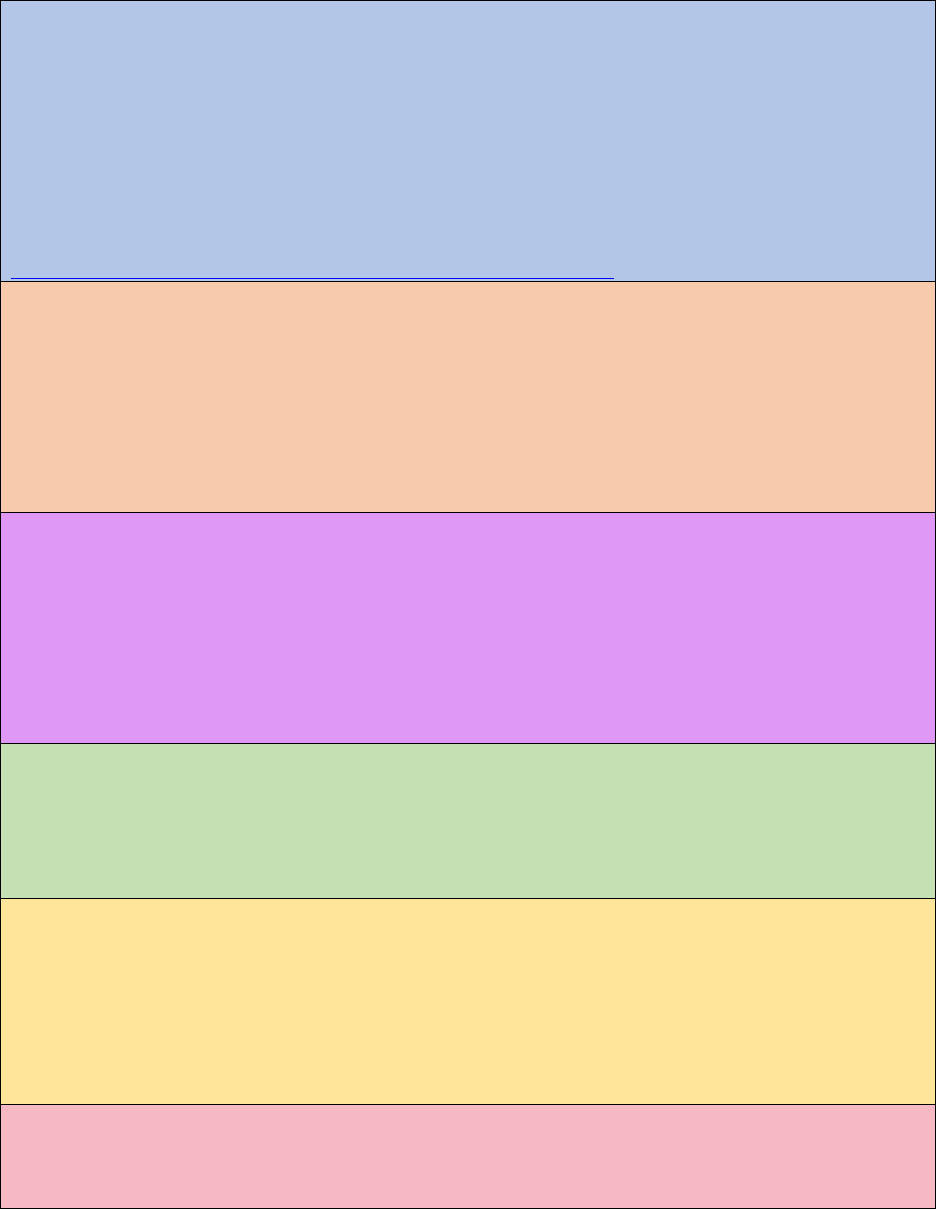
What%Can%I%do%to%Help%Maintain%My%Independence?%
'
Home%Modifications%
o Reduce#Clutter##
§ Do#you#find#yourself#losing#items#all#the#time#or#
feeling#overwhelm ed?#Clutter#around#the#house #
can#cause#many#problems.#It#is#important#to#stay#
organized#and#keep#your#home#tidy.#This#can#help#
you#to#locate#items#easier#feel#less#overwhelmed.##
#
' ' '
'
'
'
'
'
'
'
'
'
'
'
Becoming less mobile often accompanies cognitive deficits as symptoms of
Dementia progress. Other compensatory techniques could be use of adaptive
equipment including:
Adaptive
Equipment
Rationale
Price
Range
Resource Link
Bathroom
Grab Bars
This assistive device can provide
support and stability for an
individual who is confused or
agitated with an unsteady gait.
Maintaining balance during bathing
by using grab bars with textured
handles will greatly increase safety
and decrease fall risks on slippery
surfaces.
$20.00 -
$150.00
https://www.healthproduc
tsforyou.com/p-carex-
textured-wall-grab-
bars.html
Tub
transfer
bench
Poor balance may be more
prevalent in later stages of
Dementia. Individuals need extra
support to compensate for
instability. A tub transfer bench will
provide the additional support that
is necessary during bathing.
$30.00 –
$3,000.00
https://www.healthproduc
tsforyou.com/p-lumex-
imperial-collection-
transfer-bench.html
Walker
A walker can have a profound effect
on stability for individuals with
walking difficulties. Stiffness is a
common symptom of this
progressive disease making this
assistive device medically necessary.
A walker can act as a support for
functional mobility while greatly
increasing safety.
$45.00 -
$500.00
https://www.healthproduct
sforyou.com/p-graham-
field-lumex-two-button-
adult-folding-steel-
walker.html
Contrast
tape
Outlining edges of counters, steps,
coffee tables, doorways, bathtub
with contrast tape makes edges
easier to distinguish. Without
contrasts, the likelihood of falls and
accidents are increased. Contrast
tape is medically necessary to
ensure safety of individuals with
visual perceptual deficits with
Dementia.
$19.95 -
$75.00
https://www.maxiaids.co
m/low-vision-reflective-
tape-black-and-yellow-
striped

6
Mental%Exercise%
!
o There#are#many#ways#to#exercise#your#brain.#The#
following#are#good#w a y s#to #kee p #yo u r#mind#going#and#
strong:#
§ Rehearse#new#tasks#over#and#over.#The#more#you#
practice,#the#easier#the#task#will#be.#
§ Practice#mindfulness.#Take#one#task#at#a#time.#
This#will#help#you#to#focus#and#complete#one#task#
before#moving#on#to#another.##
§ Stick#to#a#routine.#Doing#your#morning#activities#
in#the#same#order#will#help#you#to#reme mber#each#
and#every#one.#You#will#less#likely#miss#a#step#the#
more#you#do#it.#
§ Engage#with#family#members.#Family#will#help#
you#through#difficult#times#and#encourage#you#to#
keep#going.#Talking#about#old#memories#can#also#
help#keep#your#mind#strong.#
§ Safety2is#important.#Make#sur e #to #talk#ab out#your#
safety#with#your#family#or#caregivers.#Have#your#
family#take#out#any#items #in#th e #ho u se #th at#may#
cause#you#harm.#2
Helpful%Resources%
• www.amazon.com##
o Use#this#website#to#purchase#items#described#above.#
Once#you#are#on#the#website,#click#in#the#search#bar#and#
type#in:#Alexa,#medication#boxes,#noteb o oks,#etc.#and#hit#
enter.##
#
• https://ocfch.org/hand-in-hand/declutter/#
o This#website#provides#a#great#explanation#and#video#on#
the#best#process #o f#de-cluttering#a#home.##
#
#
Resources
Online Tools – community resource finder: Local support groups, community programs
and resources available can be navigated through this website. Programs and events, home
care information, community services, housing options, and medical service based on your
location can be found here: https://www.communityresourcefinder.org/
Helpline phone number: This is a free 24/7 helpline through Alzheimer’s Association that
clinicians help in providing reliable information and confidential support for those who need
assistance; for the individual with AD/dementia, family members, caregivers and the public. The
helpline phone number is (800)272-3900.
Memory Loss Concerns: Guides for notetaking and directed conversations are provided for
both caregivers/family members who have noticed changes in their loved ones and individuals
who have noticed changes in themselves. These guides can be found on
https://www.alz.org/help-support/resources/memory-loss-concerns.
Caregiving assistance: Topics including understanding Alzheimer’s and dementia, driving,
doctors visits, financial planning, legal planning, and caregiver strategy program and effective
communication strategies according to stage of dementia are provided.
https://www.alz.org/help-support/resources/care-training-resources.
Further Professional Assistance
Dementia is a progressive disease and staying physically active has a big impact on the well-
being of the individual experiencing dementia. Physical, occupational, recreational, and speech
therapy could greatly assist an individual with dementia.
-Physical therapy: increase strength, endurance, and safety for
the individual; making a daily exercise program and providing
specialized care.
-Occupational therapy: help in assisting in ADLs (dressing,
bathing, brushing teeth) and provide continuous support with
compensatory strategies and adaptive equipment, including those
listed above, to increase meaningful activities quality of life overall.
-Recreational therapy: provide leisure and recreational
activities for the individual as well as assist in identifying leisure
pursuits and hobbies to promote physical activity.
-Speech pathology: assist with any speech or swallowing issues as well as stimulate
cognitive activities. As the disease progresses therapy could greatly benefit an individual with
dementia.
Improving Occupational Engagement – Further Considerations
Common symptoms for all types of dementia are initially similar; short-term memory loss,
decreased problem solving skills and decreased visual perceptual skills. Treatment approaches
relating to compensatory strategies can be applied to all the initial symptoms. Making
appointments and the same time, writing yourself reminders, and keeping a calendar are great
compensation techniques for decreased short-term memory and can help decrease the effects
of these symptoms on daily life. Reminders can influence attention, thought process, and help
to orient the individual to the experience of self and time.
Organizing a pill box can promote consistency of daily routines as using it becomes a habit,
while also providing memory compensation. Decluttering the living environment will ease
difficulty with motor and process skills such as coordination, pace, and ambulation. Having clear
walkways in the home will also increase safety and decrease fall risks. Assistive technology,
such as electronic reminders and apps, can challenge perception and thought while also being a
compensatory strategy for memory.
Lastly, during later stages of dementia adaptive equipment can help support physical deficits
including joint stabilization, gait patterns, lack of visual function, and postural reactions.
Medication use for dementia symptoms may also result in weakness. Adaptive equipment will
usually be a later modification when other compensatory techniques can no longer be
implemented. As the disease progresses more chronic physical and mental changes take place
during later stages of dementia.
Age-related Changes Related to Dementia
Affecting Occupational Performance
• Reaction time: Slower thinking process and body movements.
• Proprioception: Potential postural instability and falls; changes in joint-
position sense during movement.
• Balance: Postural control is disturbed by changes in sensory, motor, and
central nervous system function, and affected by a decrease in sensory cues
and reflexes.
• Motor activity: Posture, movement, gait, and reflexes are altered with
aging.
• Sleep disturbance: Changes in sleep patterns are commonly experienced to
people over age 65, insomnia is the most frequent aging-related sleep
complaint. Typical aging-related changes in the sleep cycle include lighter,
more easily interrupted sleep, with more time spent in the lightest sleep
stage and less time in deepest sleep. Comorbidities may affect sleep
patterns, as may medications, smoking, or napping.
References
Alzheimer's Disease Fact Sheet. (2020). Retrieved from
https://www.nia.nih.gov/health/alzheimers-disease-fact-sheet#stages
Barney, K. F., Emerita, C., & Perkinson, M. A. (2018). Cognitive Impairment, Dementia, and
Occupational Therapy Interventions. Kempf, C., Schwarz, L. R., Desai, A. K., Perkinson,
M. A. (Eds.), Occupational therapy with aging adults: Promoting quality of life through
collaborative practice. (pp. 245–265). Elselvier.
Dementia and the Role of Occupational Therapy. (2020). Retrieved from
https://www.aota.org/About-Occupational-
Therapy/Professionals/PA/Facts/Dementia.aspx
Higuera, V. & Ellis, M. (2018). 10 Early Symptoms of Dementia: Be Aware of Subtle Signs.
Retrieved from https://www.healthline.com/health/dementia/early-warning-signs
Online Home Healthcare and Healthy Living. (n.d.). Retrieved from
https://www.healthproductsforyou.com/
